A new study shows that a lack of specific bacteria in the gut stalls liver regeneration – a life-saving process in the body.
Our tummy is home to a menagerie of tiny microbes, such as viruses, fungi, and bacteria, which form our microbiome, a symbiotic entity that plays many roles in our body, including the regulation of our digestive system and immune responses. Now, a recent study by Technical University Munich (TUM) researchers suggests this omnipotent colony may also assist in liver regeneration following significant tissue loss.
Their work, involving live mice and human liver tissue, found that a lack of the bacterial species responsible for producing fatty acids in the gut stalled the rate of hepatic regeneration after part of the organ was surgically removed (resected). These findings were observed in mice who had received a course of antibiotics that caused an imbalance of microbiotic species in the gut-a state known as dysbiosis-whereupon an uncommon species took over that couldn’t produce the lipids needed to rebuild the animal’s livers.
An essential reason for this study revolves around the dichotomy of the liver’s remarkable capacity to recover from injury or a partial loss of tissue coupled with high rates of liver disease, which is still a major killer worldwide. And as experts consider inhibited hepatic regeneration the main culprit, the mechanisms responsible for this process continue to be the target of intense research, with the hope that the knowledge gained will one day lead to novel strategies to improve the outcomes of many liver diseases.
So far, metabolites produced by gut microbiota have been associated with liver disease and progression, hinting at a limited or expedited healing process. However, the effects of these microbial products on hepatic regeneration after an injury or surgery are still not fully understood. Up until now.
The new study makes a significant discovery in the field by identifying the species of gut bacteria responsible for this process. Specifically, it shows that liver regeneration comes to a standstill when there is a decrease in the Firmicutes and Bacteroidetes microbiota in the gut. These bacteria-the dominant taxa in the gut microbiome-produce an essential enzyme and the lipids needed to rebuild the liver after an injury or tissue loss. The team says these new findings could proffer a way for doctors to check that host conditions are optimal for the liver to reconstruct itself before surgery has even taken place.
“Liver cells need these fatty acids to grow and divide,” explains study leader Prof. Klaus-Peter Janssen from TUM’s School of Medicine. “We have now succeeded in showing for the first time that gut bacteria influence the lipid metabolism in liver cells, and therefore their ability to regenerate.”
Mapping antibiotic damage
Partial resection of the liver remains a mainstay for treating hepatic diseases. However, ‘insults’ to the gut microbiota, like antibiotics that cause dysbiosis, can stall the regeneration of the liver. In the past, scientists had assumed that antibiotics alone were affecting this reconstruction, but the TUM researchers hypothesized that if the antimicrobials were affecting the gut microbiota, then this native entity must also have the capacity to impair hepatic synthesis. It was now up to them to find out just how this microcosm does this.
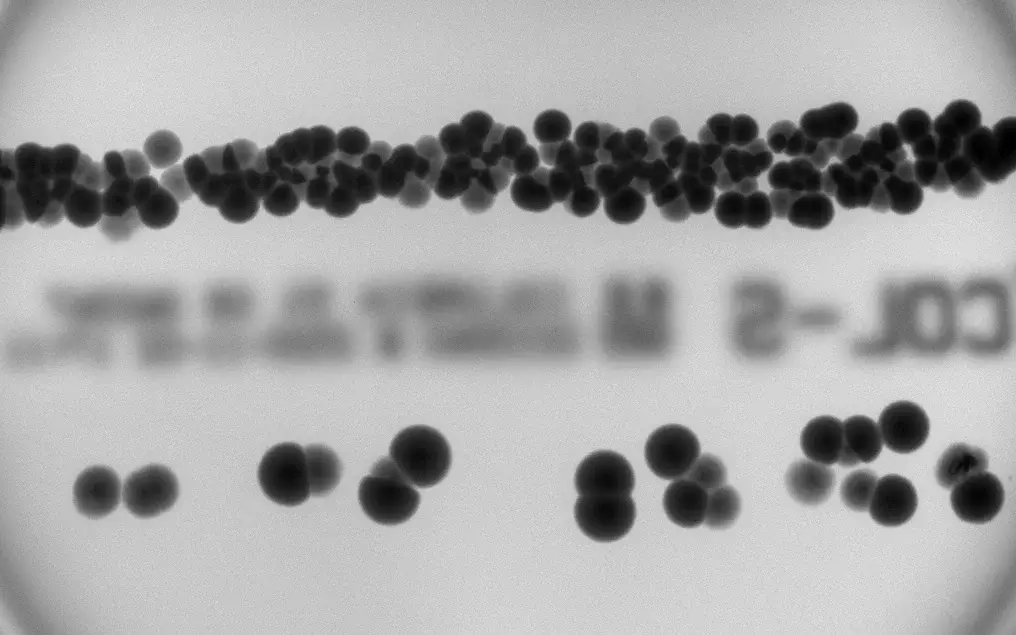
The first step was to induce dysbiosis in mice using antimicrobials. The animals, known as the antibiotics group, were compared to germfree mice bred without a gut microbiota and a control group raised under normal conditions. All three murine groups had their livers resected to stimulate the proliferation of specialized cells called hepatocytes, which make up most of the liver. The scientists determined the number of cells produced using blood tests and weighing the animals at various time stamps after surgery to establish how much the liver had grown. As these cells depend on lipids for growth and proliferation, the team was also able to firmly posit that fat cells play a large part in liver regeneration.
After three days of antibiotics, this group exhibited delayed regeneration, which recovered with the animals’ microbiomes within a few weeks. However, they didn’t produce as many hepatocytes as mice in the control group, who also propagated larger-sized cells. Startingly, in mice lacking gut bacteria, no regeneration occurred, but the researchers say they were able to kickstart the process by performing a microbiome transplant on the animals.
Essential bacteria depleted
Using cultures of fecal pellets and intestinal or cecal content, the researchers say they identified the bacterial communities or taxa present. Results show that the antibiotic treatment led to a massive increase in Proteobacteria, accompanied by decreased levels of fatty acids. In contrast, the abundance of Bacteroidetes and Firmicutes bacteria remained relatively stable in controls, while the amount of Proteobacteria remained very low.
In their white paper, the scientists explain that the Proteobacteria taxa only constitute around one percent of the healthy microbiota, with the Firmicutes and Bacteroidetes species comprising the other 90 percent. These two dominant phyla are also responsible for producing fatty acids by fermenting dietary fiber in the gut – a functionality Proteobacteria does not possess – explaining the low levels of lipids accompanying the decimation of this dominant species in the antibiotics group.
How does fat build the liver?
Using mini liver organoids made up of mouse cells in a Petri dish, the researchers demonstrated how fatty acids provide essential building blocks for the liver’s cell membranes. Their experiments showed that if there aren’t enough lipids present, the cells won’t be able to grow and reproduce. In comparison, as long as the microbiota is healthy, they can produce a fatty acid called acetate, which reaches the liver via the portal vein. Once there, it’s modified in hepatocytes by the enzyme SCD1 to produce monounsaturated fatty acids and incorporated into the liver’s cellular membranes as phospholipids – fat cells organized into bilayers.
It’s important to mention that the team found out that the SCD1 enzyme plays a vital part in liver regeneration, and its activity depends entirely on the microbiome’s state. They confirmed this by studying human tissue and observing that the enzyme’s expression increased significantly after resection, upon which antibiotics delayed its activity.
In their white paper, the team summarizes that the gut microbiota produces metabolites that promote liver regeneration through the gut-liver axis. Subsequently, insults to the microbiome, such as antibiotics, disrupt the production of these compounds needed to produce new membrane lipids in hepatocytes: impairing liver proliferation and survival after resection.
Commenting on the microbiome’s diversified roles in liver biosynthesis, Klaus-Peter Janssen says, “It is important to bear in mind that the role of gut bacteria in our bodies is highly complex. We have a long way to go before we fully understand it.” As a result, he says their study does not provide any suggestions for the development of medications. Nonetheless, he concludes that doctors can still use the results to decide if the microbiome is fit for surgery or if it’s best to delay the procedure and assist in its recovery through a specific diet.

